Inferior alveolar nerve block (IANB) is the technique that is most frequently employed to achieve local anesthesia of the posterior inferior teeth, especially in the case of endodontic procedures as well as restorative and surgical procedures in the mandibular molar teeth. However, clinical studies have demonstrated significant failure rates for this technique, indicating that IANB does not always result in successful pulp anesthesia even when it is performed by the most experienced clinician.
Concerning pulpal anesthesia, success rates with absolute IANB range from 42% to 73% for non-inflamed pulp whereas lower values are observed for irreversible pulpitis. Numerous studies have emphasized that, although all patients report lip numbness following IANB, this factor is negligible regarding the measure of the success of mandibular anesthesia. In the case of IANB, dentists normally begin treatment on their patients within 10 to 15 minutes after injection of the anesthetics. Therefore, if the symptoms of anesthesia are not identified within this period, anesthetic failure can be assumed to have taken place.
Another alternative is the use of supplementary techniques such as intraligamentary or intraosseous injections and intra-pulpal anesthesia The reasons for IANB failure are not yet fully understood. They may be due to an anxiety factor, which directly lowers the pain threshold, as well as to psychological factors such as personality and expectations, which influence the perception of pain. Also, the theory of accessory innervations of mandibular molars should not be overlooked, even though the IANB failure rate exceeds the incidence of this innervation. Additionally, the resting potential and threshold of excitability of the neurons from inflamed tissues might change, which could culminate in chemical changes that can affect anesthesia. However, there seems to be no significant correlation between failure rates and the type, concentration, and volume of anesthetic agents .
Fortunately, when local anesthesia fails, this can be managed effectively in most cases. This may involve modification of conventional techniques to overcome anatomical problems such as variations in the location of the mandibular foramen for example, the use of “high” blocks such as the GowGates or Vazirani-Akinosi techniques
Choice Of Anesthetic Agent

Anesthetics have different features in terms of latency period, potency, and action time of anesthesia. The choice of anesthetic drug depends on the type of procedure that is to be performed and on the overall health condition of the patient .
However, some studies have shown that the appropriate selection of local anesthetics is not enough to prevent transmission of nerve impulse. This is because the thresholds of excitability might be reduced .
Sodium channels resistant to tetrodotoxin might also be involved in IANB failure, since these channels have also been demonstrated to be resistant to the action of local anesthetics .
Inappropriate Technique:
As for the use of inappropriate techniques, it is important to emphasize the mandibular region. If the injection is too low, lingual anesthesia will result in deficient anesthesia of the tooth and bone structures. An injection that is applied too deep might mean that the solution will be deposited in the parotid space.
This culminates in temporary facial nerve anesthesia and paralysis, which will last until complete absorption of the anesthetic is achieved, and no anesthesia of the mandibular nerve takes place. If injection is too mesial, the solution will be deposited in the pterygoid muscle, with superficial anesthesia and trismus. In the case of an excessively superficial injection, the anesthetic solution will be superficially deposited in the pterygomandibular space (distant from the mandibular foramen), and inadequate anesthesia may occur .
An injection applied too high may result in no anesthesia, since the solution is deposited in the sigmoid condylar notch or neck. Finally, intravascular injection does not induce adequate anesthesia and may cause systemic complications It is also important to bear in mind that anatomy varies with age and development of the facial structures.
If a line tangential to the occlusal surface of the last molar is drawn, the Spixs spine (lingula or elevation near the entrance of the mandibular foramen) is localized one centimeter above this line in adults and at the level of the line in children. In edentate patients, it is important to keep the horizontal plane in mind, in order to avoid deposition of the anesthetic solution below the mandibular foramen .
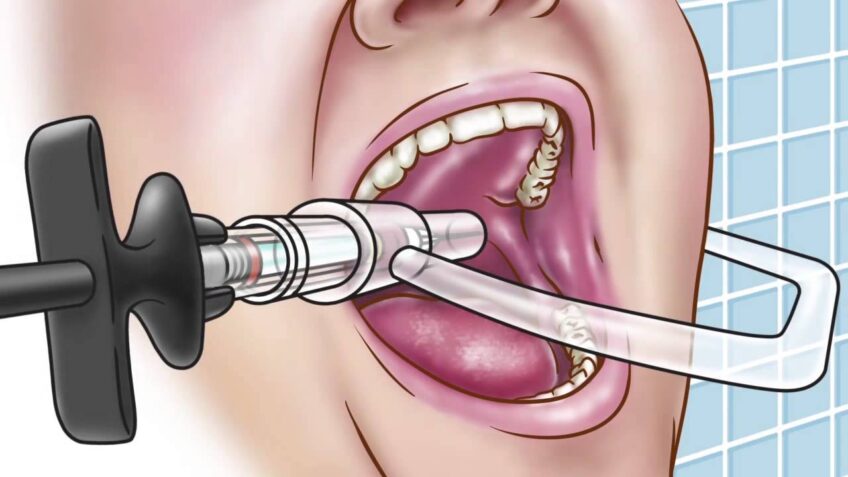
The error that is most likely to occur during the performance of anesthesia is wrong needle placement. Absence of aspiration before injection can lead to intravascular deposition of the solution, which can also cause failure of anesthesia. Successful anesthesia may be related to the speed at which the solution is deposited.
It is easy to imagine the anesthetic being directed away from a nerve trunk during a forceful injection. Indeed, there is evidence that the solution should be deposited slowly .
Practitioners who frequently fail to carry out this type of AINB should reassess their technique. The best way to achieve success is to use a direct technique, where the dentist places the thumb intra-orally at the deepest concavity of the anterior ascending ramus and the index finger at the same height extra-orally on the posterior aspect of the ramus. The point between the mid-point of the thumb nail and the pterygomandibular raphe is where the needle should be inserted.
The needle should then be advanced through this point parallel to the occlusal plane from the premolar teeth of the opposite side. The final point of the bone is achieved at a depth between 15 and 25 mm. A common error is injecting the solution below the mandibular foramen, which can be corrected by means of a higher injection.
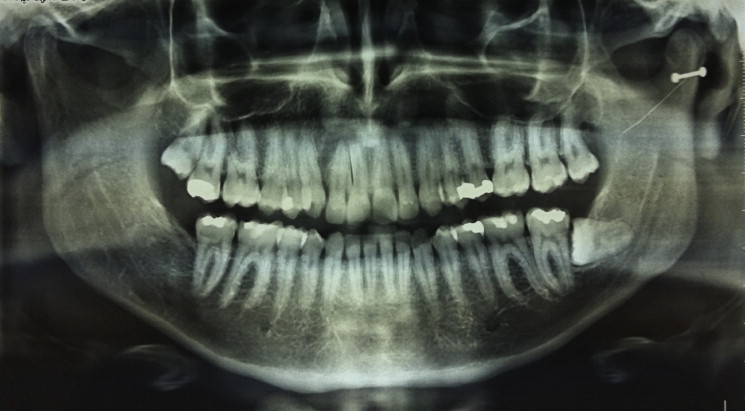
In most cases, the practitioner who has frequently failed to carry out anesthesia attempts to overcome the problem by repeating the injection. In this context, a panoramic radiograph shall help localize the position of the mandibular foramen.
The patient-dependent failures may occur because of anatomic variation, bifid alveolar nerve, bone density, retromolar foramen, accessory innervation, accessory mental foramen, and nerve anastomoses .
Anatomical variations:
With respect to anatomical variations, in this review we highlight the myloyoid nerve accessory supply. Accessory innervations of cutaneous cervical nerves, C1, C2, and auriculotemporal nerve; variations in nerve pathways; differences in the position of the foramen; bifid mandibular canal or bifid alveolar nerve; accessory mental foramen; bone density; and nerve anastomoses12 will also be discussed. The important mandibular foramen regarding regional anesthesia in anesthetic block does not have consistent location among patients.
Available radiographs may be helpful in anticipating this situation The inferior alveolar nerve is known to be located in apical and lingual position with respect to the third and second molars A greater distance from the vestibular zone to the mandibular canal has been reported to occur between the first and second molar, with vestibular displacement of the nerve taking place at the second molar level, toward the mental foramen .
A higher or lower position of the mandibular canal has been radiographically observed . Finally , the mandibular canal varies with patients age, being localized in a higher position after 60 years of age .
Mandibular foramen:
Knowledge of the precise location of the mandibular foramen (MF) is essential in dentistry for effective mandibularblock anesthesia injection and for certain other procedures in oral and maxillofacial surgery , however, it is not universally successful. A number of authors describe the position of the foramen as halfway between the anterior and posterior borders of the ramus Nicholson found in the population of 80 East Indian adult dry skulls the position of the foramen was found to be variable, thus confirming the results of previous works .
As far 36 on their study revealed that the MF can be localized in panoramic radiographs but that its relation to clinically palpable and radiographically visible bony landmarks is highly individualistic. In another study, were found statistically significant correlations between the mandibular angle position and the narrowest anteroposterior diameter of the ramus and between the distance from the deepest point of the ramus to the MF and the narrowest anteroposterior diameter of the ramus in radiographs done with the Orthoralix SD Ceph . The success of this technique is dependent on placing the needle tip in close proximity to the MF36 and it is essential to deposit the fluid as close as possible to the nerve .
Accessory mental foramen:
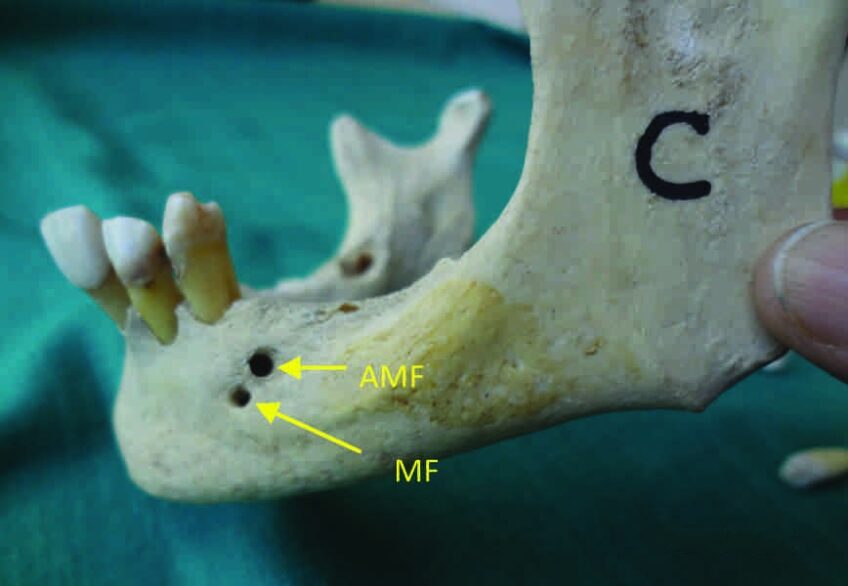
This foramen is localized apically or near the mental foramen, and it also contains mental nerve fibers However, data relative to its existence are controversial. While a study has reported a prevalence of 6.62% of the accessory mental foramen in 138 mandibles another investigation has described a much smaller percentage (2.5%) In another work, a series of 5000 panoramic radiographs failed to detect this foramen In a further study involving four population groups, the authors found a lower percentage of this anatomical variation in whites and American Indians from Asia (1.4% and 1.5%, respectively) .
Bifid inferior alveolar nerve:
The bifid alveolar nerve is a possible cause of IANB failure In 0.4% of the cases, the nerve has two or three ways via an accessory foramen, which contains small sensory nerve fibers. In a series of 6000 panoramic radiographs, it was observed that 57 (0.95%) contained a bifid channel while another study found 7 images suggestive of bifid canal in a series of 2012 panoramic radiographs .
Additionally, 33 bifid channels were identified in another group of 3612 patients (0.9%), 20 of which were bilateral and 13 were unilateral. 48 These findings indicate that the channels are not commonly bifid. Indeed, the prevalence of bifid channels is around 1% .
Bone density:
The most obvious barrier to diffusion of anesthesia is the plate thickness of the mandibular cortical alveolus, which blocks the infiltration of anesthesia in adults. The opposite is applied to children, in which the infiltrative approaches are most commonly used due to the existing low bone density . In the maxilla, the region of the first molar in adults may also present a similar problem. This is because it is a thicker zygomatic region that is sturdy enough to prevent the passage of anesthetics to the dental apices .
Retromolar foramen:
The presence of a retromolar foramen with or without the existence of a bifid mandibular nerve has been investigated. The presence of such nerve fibers was detected in the mentioned foramen Likewise, a prevalence of 7.8% of the foramen has been reported for a series of 249 African-American and 226 caucasians, without significant differences in terms of race or sex .
In a study of 234 adult mandibles, a prevalence of 7.7% of the retromolar foramen has been described, with no differences between men and women .This anatomical variation provides accessory innervation, which may cause failure during mandibular block.
Accessory innervations:
Teeth may receive innervation from more than one nerve trunk. The accessory nerve supply can lead to failure of anesthesia, including IANB. The buccal nerve may occasionally provide pulpar innervation to the inferior molars and, in this case, a buccal infiltration anesthesia might be necessary. The lingual nerve may also contribute to pulpal anesthesia of the lower teeth, but this will normally be counterbalanced by this nerve blockade in association with AINB. Other sources of accessory nerves innervate the inferior teeth. This supply may be derived from mylohyoid, auriculotemporal, and upper cervical nerves .
Several authors have emphasized that accessory innervations of lower teeth are a possible explanation for the incidence of inadequate anesthesia. The mylohyoid nerve is the best documented accessory nerve of the mandibular teeth.
The mylohyoid nerve is a mandibular branch of the trigeminal nerve that provides motor innervation to the mylohyoid and digastric muscles. However, it may also present a sensory component, providing accessory innervations and causing IANB failure .The mylohyoid branch leaves the main trunk of the inferior alveolar nerve one centimeter up the mandibular foramen . Therefore, it cannot be affected by a conventional approach.
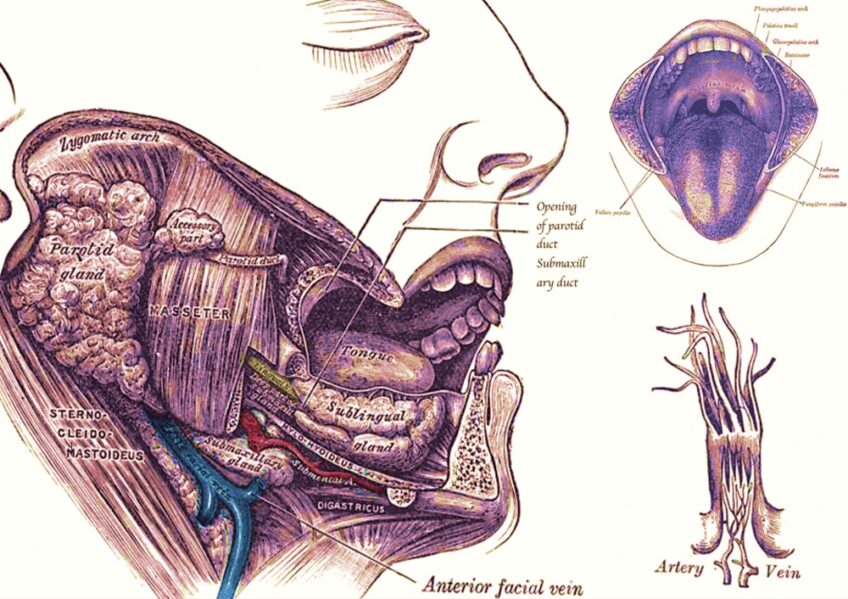
The auriculotemporal nerve has been reported to occasionally send branches to the pulps of the inferior teeth via the upper branch . This supply, such as the branch of the mylohyoid nerve, can be counteracted with a “higher” blockade, including the Gow-Gates technique and Akinosi technique. The innervation that corresponds to the first cervical branches can also be present, with fibers exhibiting gingival, bone and tooth action in the mandibular posterior region .
Anastomoses nerve:
The contralateral innervation of the anterior teeth can cause failure of anesthesia in both the maxilla and the mandible . In a study analyzing a series of 38 patients and evaluating the percentage of nerve anastomosis on the unilateral and bilateral anesthesia of the inferior alveolar nerve, the authors found that cross innervations may cause a significant number of anesthetic failures in the lateral and central incisor . This fact was attributed to the cross passage of the inferior alveolar nerve and to the accessory innervations of the oral and facial nerves and the brachial plexus . IANB failures may also be due to pathological, pharmacological and psychological causes and to problems related to the anesthetic solution itself.
Psychological causes:
Fear of seeing and/ or feeling the needle and the sound of the dental handpiece are routinely cited as causative agents in the creation of anxiety in dental patient . Several methods have been advocated for managing anxious patient pain . In any case, the clinician should establish a positive and confident relationship and avoid exposing the patient to obvious fear-producing stimuli .
Many clinicians report that a sense of humor often helps to relax apprehensive patients . Early identification of the problem, a meticulous technique, and sedation can help in these situations . For apprehensive patients who report the absence of local analgesia, the use of sedative techniques may be helpful for the success of anesthesia, since the patient will feel more relaxed .
Ineffective anesthetic solution:

Even if the technique is correctly performed, the desired effect will not be achieved if the solution is altered. Certain batches of a particular drug can be past the expiration date and therefore should not be used, or failure will result .
The storage of anesthetics at temperatures above 37ºC can also lead to failure of anesthesia, especially in the case of those available in plastic cartridges .
The injection pressure, especially in the case of intraligamentar infiltration, can culminate in cracking of the tube and thus anesthesia failure .
Central core theory of nerve block failure
The central core theory states that the nerve fibers toward the center of the nerve travel the furthest and are the last to be anesthetized . In some cases the anesthetic solution may not completely diffuse into the nerve to produce an adequate nerve block in all teeth .
This theory may be the best explanation for the failure of inferior alveolar nerve block. It states nerves on theoutside of the nerve bundle supply molar teeth, and nerves on the inside supply incisor teeth. The anesthetic solution may not diffuse into the nerve trunk to reach all nerves and produce an adequate nerve block. The theory may explain the higher failure rates in incisor teeth with the inferior alveolar nerve block.
Conclusion

Effective local anesthesia is an important aspect of dental practice. Hopefully the reader has found this review to be informative and practical. Our objectives were to review the probable causes to inferior alveolar nerve block failure in order to help the clinician to achieve a higher success rate of inferior alveolar nerve block.

